Abstract
Introduction: Thymus and activation-regulated chemokine (TARC) has been recently identified as a promising predictor of response in patients (pts) with classical Hodgkin's Lymphoma (HL). A correlation between treatment response and early sTARC reduction in HL pts treated with PET-adapted strategy was reported (Guidetti A, Leuk Res, 2017; Viviani S, Hematol Oncol, 2020). In the current study, we analyzed the kinetic of sTARC in HL pts during first-line treatment, with the aim to evaluate its potential predictive value.
Methods: We prospectively collected plasma samples of naïve HL pts. Pts were stratified according to GHSG risk categories. Localized HL were treated with 2-4 cycles of ABVD followed by involved field radiotherapy (IFRT); advanced HL underwent 6 cycles of ABVD. Pts with a positive PET-2 switched to an intensification treatment. Pts with positive end of treatment PET (EOT-PET) were treated with BeGEV followed by autologous stem cell transplantation (ASCT).
sTARC levels were measured with a commercial TARC ELISA kit (R & D Systems, Minneapolis, US) according to manufactory instructions. Samples were collected immediately before treatment on day 1 of each ABVD cycle, before IFRT in localized stages, on day 1 of each cycle of salvage therapy, including ASCT, and 1 month after EOT. Samples were analyzed in duplicate. Statistical analysis was performed using IBM SPSS Statistic v.27 and GraphPad PRISM v.8; Continuous variables were compared by Mann-Whitney U test, categorical variables by χ 2 test. Statistical significance was defined as P=.05.
Results: Of 43 pts enrolled in the study, 4 pts were excluded due to missing samples, and for 3 PET-2 positive pts data were unavailable at time of this analysis; overall evaluable pts were 36. Median age was 33.5 yr (range 17−65), 58% pts were male. B-symptoms were present in 50% of pts. Fourteen pts (39%) were early stage (IA, IB, IIA), 22 pts (61%) were advanced stage (IIB, III, IV). Four pts (11%) were refractory, documented by EOT-PET positivity. For the purposes of this analysis, pts were stratified in two subgroups including stage I pts (11%) and stage II-IV (89%).
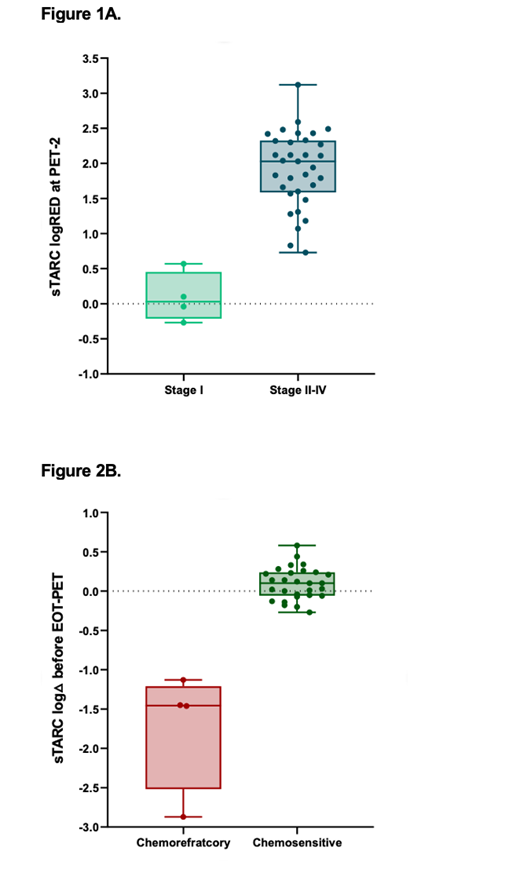
Median baseline sTARC was 35,454 pg/ml (range 273−183,225); levels were significantly lower in stage I compared to stages II-IV (524 vs 50,606 pg/ml, P=.001). Median sTARC after 2 ABVD cycles (sTARC-2) was 482 pg/ml (range 97−2,071) in the whole population, with a median logarithmic reduction (logRED) vs baseline of 1.83 (range -0.26−3.12). In stage II-IV a significant decrease of sTARC-2 (median 493 pg/ml; range 97−2,071), with a median logRED of 1.94 (range 0.73−3.12), was observed, unlike in stage I where sTARC-2 remained stable (median 393 pg/ml; range 279−805); median logRED -0.03 (range -0.27 to 0.57) (Fig 1A).
We then compared sTARC in chemorefractory and chemosensitive stage II-IV pts. We observed an almost significant difference (P=.077) by considering baseline sTARC in the two groups, respectively 95,236 pg/ml (range 53,502−135,787) in chemorefractory and 35,454 pg/ml (range 5,475−183,225) in chemosensitive pts. However, sTARC-2 and the logRED of sTARC-2 were not significantly different between the two groups: 654 pg/ml (range 97−1,564) vs 463 (range 150−2,071) and 2.1 (range 1.6−3.1) vs 2.0 (range -0.7−2.6), respectively.
Finally, sTARC measurements after PET-2 and before EOT-PET, and their log variation (logΔ) as compared to sTARC-2, were assessed in chemorefractory and chemosensitive subgroups. In refractory pts, a progressive increase of sTARC was observed: median sTARC was 32,202 pg/ml (range 14,362−71,807) at the time of biohumoral relapse compared to 373 pg/ml (range 166−1,102) in responding pts (P=.001). The corresponding log∆ values were -1.5 (range -2.9 to -1.1) and 0.1 (range -0.3−0.6) (P=.001), respectively (Fig 2B).
Conclusions: The current study, with the limitations of small pts number, provides an analysis of sTARC prognostic implications in pts with HL. While sTARC is of limited value in pts with stage I disease, the kinetic of sTARC variation in pts with stage II-IV HL resulted well correlated with treatment response as assessed by EOT-PET. Specifically, an increase of sTARC during treatment after sTARC-2 may predict refractoriness at later cycles. Larger studies are needed to confirm that monitoring of sTARC in stage II-IV HL during treatment might provide prognostic and therapeutic insights.
Supported by Legato Zottola, University of Florence
Puccini: Takeda: Membership on an entity's Board of Directors or advisory committees. Vannucchi: BMS: Honoraria, Membership on an entity's Board of Directors or advisory committees; Incyte: Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; AbbVie: Membership on an entity's Board of Directors or advisory committees. Nassi: Incyte: Consultancy; Takeda: Consultancy; Roche: Consultancy; Kyowa Kirin: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal